Glycative stress and Anti-aging
Glycative Stress and Skin Aging
Glycative Stress and Skin Aging
Skin structure and functions
As the outermost part of the body, the skin protects internal parts of the body from external environment elements including impact, temperature, ultraviolet rays, and chemicals. The skin is composed of three layers: epidermis, dermis and subcutaneous adipose tissue (this list starts from the outermost layer).1)
The epidermis is the outermost skin layer with an average thickness of 0.2 mm. This layer can be further subdivided into 4 layers: stratum corneum, granular cell layer, prickle cell layer and basal cell layer (this list starts from the outermost layer) (Figure 1). The stratum corneum, the outermost layer, is water-repellent and protects the muscles, nerves, blood vessels and other organs inside the body against external injuries, and at the same time prevents bacteria, virus, etc. from entering the body. Thus, the stratum corneum plays a crucial role in maintaining the body. As much as 95% of the cells that constitute the epidermis are keratinocytes, which divide themselves at the lowermost layer of the epidermis and then migrate to the outer layers as they mature. The basal cells divide themselves, generate daughter cells and are eventually shed off from the epidermis (desquamation) over the course of 40 to 56 days, and this period is called the “turnover time”.2-3)
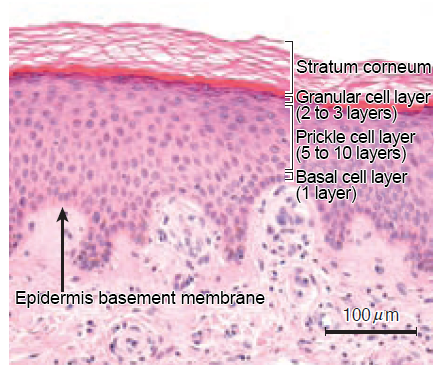
Figure 1 The four layers that constitute the epidermis
Adapted from Shimizu Hiroshi (2011)1)
The stratum corneum is a membrane tissue composed of about 10 layers of cells with no nuclei, and through exfoliation, they are shed off from the epidermis as dead skin cells one after another. The stratum corneum consists of keratin, lipids and other various constituents that the keratinocytes produce. Keratinocytes divide at the basal cell layer, differentiate and mature while producing keratin, and migrate to the upper layers. The basal cells produce keratin 5 and keratin 14, while the prickle cell layer and granular cell layer produce keratin 1 and keratin 10.
Inside the epidermis are melanocytes, which produce skin-darkening pigments, Langerhans cells, which are involved in skin immunity functions, and Merkel cells, which are tactile receptor cells.
The dermis is a layer tissue with a thickness of 2.0 to 3.0 mm and is separated from the epidermis by the basement membrane. Anatomically, the layer consists of 3 layers: papillary layer, subpapillary layer, and reticular layer. The dermis is the source of skin’s elasticity and firmness.
The dermis consists of the stromal component (extracellular matrix), which constitutes the fibrous tissue, cells that produce the stromal component (extracellular matrix), etc. The main constituents of the stromal component are collagen fibers (mainly, type I and type III collagens), elastic fibers (elastin fibers), proteoglycans (hyaluronic acid, chondroitin sulfate, etc.), etc.
Collagen represents 70% of the dry skin weight of the dermis and provides the skin with firmness. Elastin, which accounts for 1 to 2 % of the dry skin weight, is cross-linked and provides the skin with elasticity. Proteoglycans form heavily-hydrated gels and provide the skin with hydration. In addition to the above, the dermis has nerve endings for feeling the touch, comfortability and temperature, and secretory glands for adjusting the temperature of the body and for hydrating the skin to keep it flexible (sweat glands, sebaceous glands), hair follicles, blood vessels, etc.
The subcutaneous tissue is a fat layer under the dermis and has a thickness of several millimeters, although the thickness is different depending on the part of the body. The function of the tissue is to protect the body from external heat, the cold and from impact, where the tissue acts as a cushioning agent. Additionally, the adipocytes in the subcutaneous tissue store fat and act as an energy storage site.
Aging of the skin
- Deterioration of “how old you look”
When people judge the age of a person from their appearance, the sources that provide an answer to that tend to be the person’s wrinkles, skin firmness, sagging skin, color tone, radiance, skin texture, etc.4) How old someone looks will not always be the same as their chronological age. People that are of the same chronological age will look like they are different ages, after being influenced by their living environment, lifestyle habits, eating habits and other factors. The signs of aging show up most often on parts of the body that are exposed to the outside environment. An example of this would be the face. People who appear older than they actually are at a higher risk of arteriosclerosis.5) - Deterioration of skin texture
The skin surface has a texture composed of the sulci cutis, which are grooves running in all directions on the skin and extends radially from the pores in the center, and the cristae cutis (elevated areas), which are surrounded by sulci cutis. The skin texture of young people is finer and has a structure with clear and well-ordered ridges and grooves, which form the fine skin texture that feels delicate. However, the sulci cutis (grooves) become shallow and unclear with aging as the pores become larger, and the skin texture becomes less fine. The skin will look and feel rough and sandy, and the person will look older than their chronological age. - Increase in wrinkles
Wrinkles are morphological changes of the skin at a level more macro than changes in the skin texture. Wrinkles begin to appear around the eyes and mouth, and on the forehead and neck from around when people turn 30.6) The number and depth of wrinkles increase with aging. The formation of wrinkles on the face and neck are connected to the movement of muscles and the exposure to the sun. The fibers of the skin tissue are fractured by ultraviolet rays, which leads to a loss in their flexibility and a decrease in the resilience against deformation. - Change in the color tone, increase in dullness
The color tone of the skin is determined mainly by melanin (brown), carotene (yellow) and hemoglobin (red or blueish red). Light reflection and absorption change the skin tone as well due to the thickness of the stratum corneum and the condition of the skin surface (skin texture and wrinkles). Changes in the color tone of the skin due to aging include a decrease in redness, an increase in yellowness and a decrease in brightness. On the whole, the color tone of the skin will look dull.7) The factors that affect the dullness of the skin are pigmentation, a reduced blood flow rate, thickened stratum corneum, and glycation and oxidation of skin proteins. - Deterioration of skin functions
The rate of proliferation of basal cells in the epidermis decreases as the aging process progresses. The dermis becomes thinner and its turnover time longer.8) The fibroblasts of dermis will lose some of its proliferation capacity as well as some of its synthesis abilities for its matrix components. As a result, the dermis atrophies and the skin becomes less firm. One of the factors in the reduction of the cell functions is a change in the hormones, growth factors, etc. that make them insufficient in exerting their effects on the skin cells. Some factors that change the skin functions are a longer recovery time for the barrier function in the stratum corneum, a reduction in the water retention function (dryness), a change in the amount of sebum secretion due to changes in sex hormone secretion, a reduction in skin blood flow rate, and a change in the metabolism of lipids and carbohydrates.
Glycation and aging of the skin
Collagen and elastin, which are the main components of the dermis, have a long half-life period and that makes them subject to the influences of glycation.9-10) Normally, collagen and elastin form cross-linking fibers in the tissue during the process of forming fibers, via lysine and hydroxylysine residues. However, the progression of glycation in the skin tissue induces the formation of CML in the lysine residues of proteins, and cross-linking via lysine is inhibited. Thus glycation greatly affects the stability of the skin fiber tissue. Solar elastosis refers to the state where the dermis is exposed to sunlight and aberrant elastin fibers have accumulated. This is believed to occur due to the glycation of facial elastin after being exposed to ultraviolet rays for a long period of time. Symptoms of solar elastosis occur in varying degrees to all healthy people aged 30-40 or older, and it is involved in the formation of wrinkles and sagging skin on the face. In an examination of healthy subjects, their facial skin was stained with anti-CML antibodies. It was shown that the accumulation of CML in elastic fibers begins in people in their 30s and 40s. Then, the accumulation of CML expands to all elastin fibers once they are in the elderly age range (Figure 2).11) CML-modified elastin is not easily degraded by neutrophil elastase, and causes an increase in the aggregation level and the fiber’s diameter, as well as a decrease in the elasticity and the elongation rate. Thus, the glycation of elastin is a cause of skin aging.
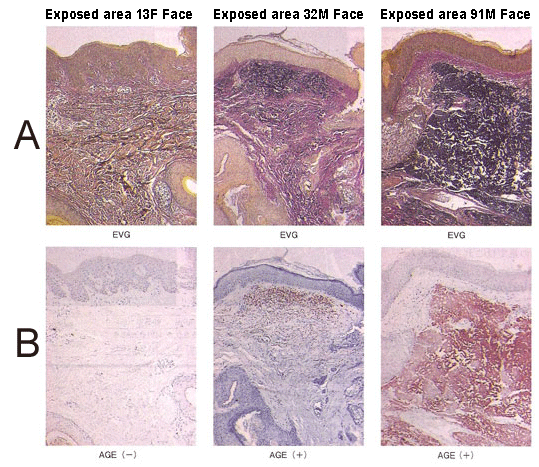
Figure 2 CML accumulation in the skin due to aging and exposure to the sun
A: Elastica van Gieson (EVG) staining,
B: Anti-CML antibody staining
The areas stained in black in the images in A indicate elastin (elastic fibers).
The darker stained areas in the images in B indicate the accumulated CML.
Adapted from Shingo Tajima (2013)11)
On the other hand, the skin shows an accumulation of AGEs in the epidermis, which has a rather short turnover period. CML accumulates in keratin 10 within the epidermis (Figure 3).12)
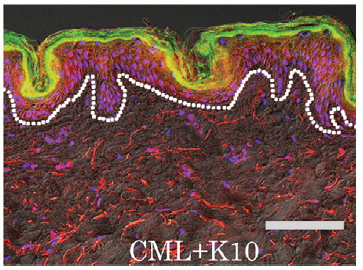
Figure 3 An accumulation of CMLs in the epidermis
Stained images of the skin tissue (71-year old female, abdomen)
K10: cytokeratin 10
CML (red: anti-CML antibody staining)
+K10 (green: anti-K10 antibody staining)
=> synthesized image (yellow)
Adapted from Kawata K, et al (2011)12)
An accumulation of CML is observed in the stratum corneum as well, which is the outermost layer of the skin. The part of the stratum corneum where a lot of CML has accumulated is where the skin texture has declined (Figure 4).13) As the accumulation of CML in the stratum corneum is related to the decline in the isotropy of the grooves on the skin surface and the decrease of the arithmetic roughness parameters, it is considered to be involved in the changes that occur to an aging face. While the increasing accumulation of CML in the stratum corneum is related to the decrease in the skin elasticity, it is correlated to the accumulation of fluorescent AGEs in the skin.
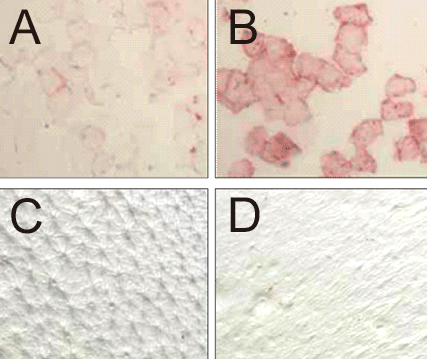 Figure 4 Accumulation of AGEs in the stratum corneum
Figure 4 Accumulation of AGEs in the stratum corneum
A, B: anti-AGEs antibody staining
C, D: replica images of the skin surface
A, C: images of the same test subject (different from B, D) who has less AGEs in the stratum corneum
B, D: images of the same test subject (different from A, C) who has more AGEs in the stratum corneum
Adapted from Takamasa Gomi (2011)13)
References
-
- 清水宏:新しい皮膚科学 第2版, 2011, 中山書店.
- Halprin KM, et al. : Br J Dermatol 1972 ; 86 : 14-19.
- Iizuka H, et al. : J Dermatol Sci. 1994 ; 8 : 215-217.
- 山田秀和:見た目のアンチエイジング, 2011, 文光堂.
- Kido M, et al. : Geriatr Gerontol In 2012 : 12 : 733–740.
- Ichihasi M, et al. : Anti-Aging Medicine. 2011 ; 8 : 23-29.
- 小澤達也:エイジングの化粧学. 1998, 早稲田大学出版部.
- Baumann L : J Pathol. 2007 ; 211 : 241-251.
- Dyer DG, et al. : J Clin Invest. 1993 ; 91 : 2463–2469.
- Mizutani K, et al. : J Clin Invest. 1997 ; 108 : 797–802.
- 多島新吾:アンチエイジング医学. 2013 ; 8 : 35-41.
- Kawabata K, et al. : Biochimica et Biophysica Acta. 2011 ; 1814 : 1246–1252.
- 五味貴優:BIO INDUSTRY. 2011; 28 : 20-26.
- 八木雅之ら:第14回日本抗加齢医学会総会要旨. 2014.
Glycative stress and Anti-aging
- What is glycative stress?
- Glycative stress biomarker measurement method (1) Measurement of blood glucose, glycated protein and glycation reaction intermediate
- Glycative stress biomarker measurement method (2)AGEs measurement
- Glycative stress biomarker measurement method (3) Evaluation of anti-glycative effects
- Glycative Stress and AGEs Receptors
- What is kidney disease?
- Glycative Stress and Skin Aging
- Glycative stress and arteriosclerotic disease
- Glycative stress and schizophrenia
- Glycative stress and liver disease
- Glycative stress and infertility
- Glycative stress and Alzheimer’s disease
- Glycative stress countermeasures (1) Blood glucose control
- Glycative stress countermeasures (2) Inhibition of glycation reaction
- Measures against glycative stress (3) Degradation and excretion of AGEs
- Measures against glycative stress (4) AGEs contained in food
- Issues and prospects of glycative stress countermeasures